Key Takeaways
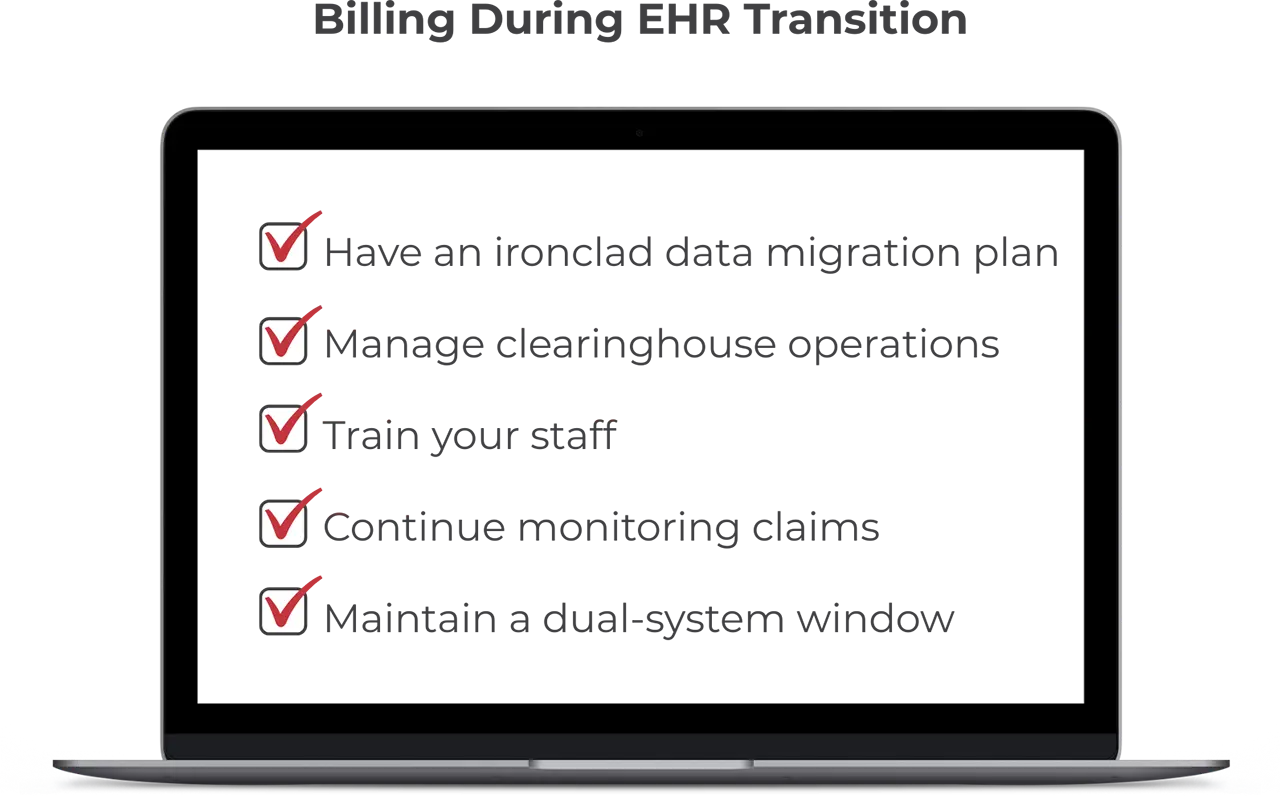
- Accurate data migration during a cardiology EHR switch prevents denied claims and payment delays.
- Clearinghouse transitions can cause cash flow disruptions if mishandled.
- Proper staff training reduces billing errors and ensures revenue continuity.
- Explore our cardiology-specific intelligent EHR features.
Billing errors are among the most common pitfalls during a cardiology practice management software transition. From clearinghouse disruptions to lost financial data, these issues can severely impact your revenue cycle. Here are five cardiology billing mistakes to avoid when switching to a new system.
Table of Contents
1. Forgetting Data Migration and Validation Steps
One of the biggest risks during a cardiology EHR transition is failing to migrate billing data accurately. Lost or corrupted financial records can lead to claim denials, payment delays, and incorrect patient balances. Research on data migration projects found that nearly 38% run over budget or experience significant delays due to errors, making careful planning essential.
How to Avoid It
Work closely with an experienced cardiology EHR vendor to develop a structured data migration plan. Before going live, validate all transferred billing data, test claim submissions, and cross-check financial records to ensure accuracy. Running a limited number of submissions in the new system before full implementation can help identify errors early.
2. Ignoring Clearinghouse Transitions
Switching to a new cardiology software system often means transitioning to a different clearinghouse. This change affects how claims are submitted and processed. If payer enrollments are not updated, or if there’s a misalignment between your clearinghouse and your EHR, you could face delays in reimbursement processing, rejected submissions, and a disrupted revenue cycle.
Clearinghouse changes can also affect Electronic Remittance Advice (ERA) and payment postings. If not managed correctly, these issues can lead to lost payments or increased administrative work for your billing staff. The American Medical Association reports that disrupted health information exchanges during EHR changeovers can create obstacles to communication and data flow.
How to Avoid It
To prevent claim submission delays, notify payers about your system change in advance and update all clearinghouse enrollment details. Your new EHR vendor can help ensure a seamless integration between the clearinghouse and your cardiology billing workflows. Build in time to monitor initial claim submissions closely to prevent disruptions and have contingency billing workflows in place in case of processing delays.
3. Insufficient Training for Cardiology Billing Staff
EHR transitions are infamous for being highly disruptive and affecting clinician and staff experiences, highlighting just how essential user education is. Even with the most advanced cardiology software, gaps in staff training can make critical claim mistakes. A lack of familiarity with the new system can lead to coding mistakes, missed modifiers, and incomplete claims—all of which can cause denials and delayed reimbursements.
Billing errors impact revenue, of course. They can also create compliance issues. Incorrectly submitted claims may result in audits or penalties, especially for services billed under Medicare, Medicaid, or private payers with strict documentation rules.
How to Avoid It
Schedule specific team preparation sessions before, during, and after implementation for all billing and administrative staff. Focus on hands-on practice, provide detailed guides, and establish a support system for questions. Encourage ongoing education, especially for areas like heart and vascular billing compliance and claim resubmissions. Designate super-users who can assist colleagues with troubleshooting as they adapt to the new system.
4. Failing to Monitor Claims When Switching EHRs
When cardiologists switch EHRs, billing teams often focus on setup and forget about monitoring billing submissions. This lack of oversight can cause backlogs, overlooked denials, and an increase in denials that go uncorrected.
How to Avoid It
Designate cardiac billing staff to track submissions in both the old and new systems for at least the first few months after switching systems. Run dual reports comparing claims data before and after migration. Use analytics tools to flag discrepancies early and ensure claims are processed efficiently.
5. Skipping a Dual-System Window
Shutting down your old EHR system too soon can create billing gaps, leading to lost revenue and compliance challenges. Without access to historical billing data, troubleshooting errors becomes difficult, and your practice may struggle to submit accurate claims.
A dual-system period allows your team to compare records, ensure billing continuity, and identify any missing data before fully committing to the new platform. Without this overlap, small errors can snowball into major financial setbacks.
How to Avoid It
Plan for a overlap period of at least 60–90 days after switching to a new cardiology-specific EHR. This transition time ensures staff can cross-check billing records, follow up on outstanding claims, and adjust to new workflows without losing revenue. If your old system allows for limited access, retain historical billing records for an extended period to support audit requests and claims reconciliation.
“Since I started working with WRS Billing Services… my patient collections over 90 days have dropped 64%, and my claim rejection rate has dropped 75%. I now have 2 more providers, and 1 PA. I also have more time to pursue activities that interest me.”
Ashish Parikh, MD, Heart & Vascular Clinic
Experience a Smooth Transition
Switching to a new cardiology software system doesn’t have to disrupt your revenue cycle. By avoiding these five common billing mistakes, your practice can maintain financial stability and ensure a smooth transition. Careful planning, staff training, and ongoing monitoring will help you maximize the benefits of your new system while minimizing billing-related risks.