Key Takeaways
- Cardiology billing and coding errors are predictable and preventable.
- Revenue should flow through a pipeline, not cycle endlessly in rejections and resubmissions.
- Rooting out the causes of claim rejections is key for optimizing cardiology revenue.
- Find out what you need to switch to the best cardiology EHR.
Running a cardiology practice means balancing patient care with the complexities of billing and collections. When your billing pipeline is inefficient, it creates bottlenecks that slow cash flow, frustrate staff, and impact the financial health of your practice. By streamlining your cardiology medical billing and coding, you can reduce errors, shorten reimbursement timelines, and ultimately boost revenue.
Cardiology practices face increasing pressure to show up for focused patient care while tackling administrative and financial demands. When billing processes stall, cash flow slows, staff frustration rises, and practice growth can be stunted. The good news is that many billing challenges are fixable—studies show that 63% of denied claims are recoverable when practices take a proactive approach. By optimizing your cardiology billing pipeline and intentionally integrating smart AI tools, you can reduce costly errors, recover lost revenue, and ensure the long-term financial health of your practice.
In this article, we’ll explore cardiology billing and coding, identify common challenges, and share strategies for creating a smoother revenue stream.
Table of Contents
Rethinking the Revenue Cycle in Cardiology
- Are your services being billed fully, correctly, and without delay?
- Do you have visibility into which cardiology procedures generate the highest revenue?
- Can you identify where claims are getting stuck?
If the answer is “no” to any of these, it’s time to strengthen your billing pipeline.
Reducing Claim Rejections in Cardiology Medical Billing
Instead, your cardiology practice should:
- Verify insurance eligibility and demographics before appointments using digital tools.
- Collect prior authorization for procedures such as stress testing, echocardiograms, or angioplasty in advance.
- Use automated eligibility checks to prevent front-end mistakes from reaching the payer.
The more proactive you are, the fewer denials you’ll face, and the smoother your revenue pipeline will run. By leveraging AI tools within your EHR, your practice can keep claim rejection rates under 2.5% by identifying and resolving issues before they reach the payer.
Clean Claims Through Accurate Cardiology Billing and Coding
Clean claims form the backbone of a healthy billing system. Strong documentation contains complete and accurate information with all necessary details included. Proper medical coding and adherence to submission guidelines ensure payers process claims without delays.
- Pair diagnoses (e.g., arrhythmia, heart failure) with the correct CPT and ICD-10 codes.
- Apply modifiers correctly when multiple cardiovascular procedures are performed together.
- Keep coding guidelines updated as payers adjust coverage for advanced imaging or device-related services.
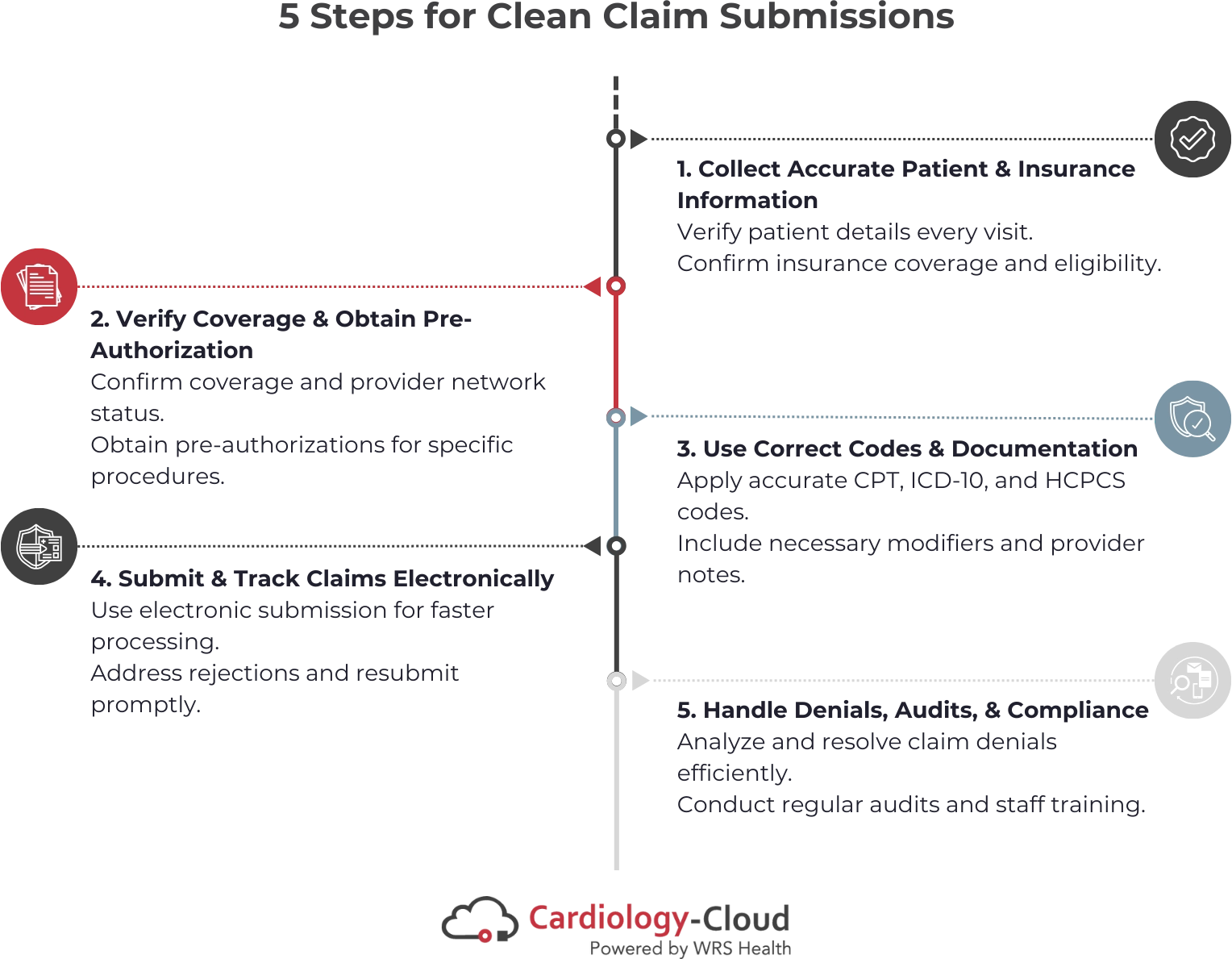
5 Steps for Clean Claim Submissions in Cardiology
1. Collect Accurate Patient & Insurance Information
- Verify patient demographics and insurance details at every visit.
- Confirm coverage and eligibility for cardiology-specific services such as stress testing, echocardiograms, or catheterizations.
2. Verify Coverage & Obtain Pre-Authorization
- Confirm plan coverage and ensure the provider is in-network.
- Secure pre-authorizations for high-value cardiology procedures (e.g., angioplasty, imaging, electrophysiology studies) to avoid costly delays.
3. Use Correct Codes & Documentation
- Apply accurate CPT, ICD-10, HCPCS, and modifying codes for cardiology diagnoses and procedures.
- Ensure provider notes fully support medical necessity for each service.
4. Submit & Track Claims Electronically
- Use electronic claim submission to accelerate processing.
- Monitor payer responses and resolve any rejections quickly to maintain steady cash flow.
5. Handle Denials, Audits, & Compliance
Review denied cardiology claims quickly, identify the cause, and take steps to prevent the same issue from happening again.
Perform regular audits and train staff so your team stays accurate, compliant, and up to date with billing guidelines and payer policies.
Staying Consistent for Long-Term Stability
Sustainable billing success requires consistent oversight. Regularly reviewing denial trends, days in accounts receivable, and payment timelines helps practices anticipate issues before they become financial risks.
Partnering for Efficient Cardiology Billing
Technology can play a major role here. Integrated EHR and practice management systems designed for cardiology streamline everything from charge capture to denial management. And if managing billing internally feels overwhelming, engaging with complete cardiology billing and coding services, like those offered by Cardiology-Cloud, can reduce administrative burden while increasing claim success rates.